Morningside Chats Hosted by Sondra Kronberg
| Join us this week! PLEASE FORWARD AND OFFER THIS RESOURCE TO PATIENTS & colleagues to add to their support - It is a completely collegial, non-competitive, non-promotional joint effort by experts. |
| Sondra Kronberg hosts: Join COPE’s own: Dr. Karen Samuels, Ph.D., Co-Founder of COPE- MARCH 11TH, 2023 CLICK TO REGISTER and/or Visit our website! Choose Support • Choose Connection • Choose Recovery Wishing you and your loved ones the best of health. Breathe and stay in each moment with love and care for yourself. ️ In honor of all of our patients and in memory of our dear friend Lynn Grefe, CEO of NEDA  • Choose Recovery Amazing Expert Guest List: Join COPE’s own: Dr. Karen Samuels, Ph.D., Co-Founder of COPE- MARCH 11TH, 2023 |
| For previous chats, newsletters and takeawaysvisit our website! |
| CLICK TO REGISTER and/or Visit our website! |
EXPERTS in the eating disorder field, iaedp, and gurze/salucore resources have come together weekly to offer free support to all clients who are struggling with this forced change in their lives and in their treatment. Morningside Chats in the Living Room is a safe space for anyone to join, listen, comment, be present and as anonymous, as you choose. Each week a different expert in the eating disorder field will engage in casual dialog and offer tips and support. Professionals are sharing their unique perspectives on life, joy, daily struggles, and the rapidly changing environment we all find ourselves in today. Morningside Chats offers a genuine source of connection and support for both the speakers and participants during this time of isolation. It is a place to connect, share, process, and uncover the silver linings or just hang out. Amazingly, professionals as well as patients are participating as a way to stay connected. Patients will be able to maintain their anonymity by signing on as anonymous in their profile or by changing their name on the screen when they sign on to the call. They will not be seen as all videos will be turned off except for those of the hosts. Professionals welcome as well!! We hope you can join us!! Best Regards, Morningside Chats in the Living Room Contact: [email protected] |
CEDO: Collaborative Eating Disorders Organizations #eatingdisordersawarenessweek2023
In honor of #eatingdisorderawarenessweek , the Collaborative of Eating Disorders Organizations (CEDO) wanted to share information about our free and accessible services that we provide throughout the U.S.
Make sure to check out all the programming that our organizations offer.
This #EatingDisordersAwarenessWeek , with the theme IT’S TIME for CHANGE, it is imperative that we come together and unite with the common goal to provide more for the community.. More equity, access, Outreach, early-intervention, education, advocacy, and awareness. We are so much stronger together! #EDAW#ItsTimeForAChange
A Proclamation for National Eating Disorders Awareness Week 2023
FEBRUARY 24, 2023
National Eating Disorders Awareness Week, 2023
- PRESIDENTIAL ACTIONS
- https://www.whitehouse.gov/briefing-room/presidential-actions/2023/02/24/a-proclamation-on-national-eating-disorders-awareness-week-2023/
Nearly 1 in 10 Americans are expected to develop an eating disorder in their lifetime. When left untreated, eating disorders can have devastating effects on a person’s health. Each of us has the power to help people who are struggling to receive the support and treatment they need and to promote a culture that treats everyone with dignity and respect. During National Eating Disorders Awareness Week, we call attention to this serious health condition and reaffirm that, with early access to treatment and support, a full recovery is possible.
My Administration is taking action to address eating disorders. Through the National Institute of Mental Health, we are working to develop better therapies and interventions. Through the Substance Abuse and Mental Health Services Administration (SAMHSA) and funding for the National Center of Excellence for Eating Disorders, we are also helping health care providers, families, caregivers, and community members access new tools and trainings to help detect and treat eating disorders.
I made tackling the mental health crisis a key pillar of my Administration’s Unity Agenda, and since coming into office, I have invested billions of dollars to improve access to mental health services. For example, we are expanding Certified Community Behavioral Health Clinics, which deliver 24/7 mental health care to millions of Americans, regardless of their ability to pay. We are also shaping brighter futures for the next generation by helping schools hire more counselors, social workers, and nurses; expanding training for health care professionals; integrating mental health into primary care; strengthening enforcement of mental health parity laws; and addressing the harms of bullying and social media platforms that fuel eating disorders, depression, and self-harm.
This week, let us acknowledge the families of those struggling with eating disorders as they care for their loved ones. Let us recommit to celebrating and supporting our fellow Americans who are on their road to recovery. And let us spread the word that help is just a phone call away: The SAMHSA National Helpline at 1-800-662-4357 is a confidential, free, 24-hours-a-day, 365-days-a-year information and referral service. For anyone experiencing a crisis, immediate and confidential help is also available by calling or texting 988, the National Suicide and Crisis Lifeline.
NOW, THEREFORE, I, JOSEPH R. BIDEN JR., President of the United States of America, by virtue of the authority vested in me by the Constitution and the laws of the United States, do hereby proclaim February 26 through March 4, 2023, as National Eating Disorders Awareness Week. I encourage citizens, government agencies, private businesses, nonprofit organizations, and other interested groups to join in activities that will increase awareness of what Americans can do to prevent eating disorders and that will improve access to care and other support services for those currently living with an eating disorder.
IN WITNESS WHEREOF, I have hereunto set my hand this twenty-fourth day of February, in the year of our Lord two thousand twenty-three, and of the Independence of the United States of America the two hundred and forty-seventh.
JOSEPH R. BIDEN JR.
We’ve Got the POWER: #EDAW
Eating Disorders Awareness Week 2023: Embodied Empowerment Movement Groups
Free | On-Demand Events
https://renfrewcenter.com/events/eating-disorders-awareness-week-2023-powering-up-together/
Two Options Available: Standing/Active Group & Seated/Low-Impact Group
NOT ONE MORE Weekend
FEBRUARY 24, 2023
- FEBRUARY 26, 2023
NOT ONE MORE Weekend
We are thrilled to announce NOT ONE MORE Weekend, Friday, February 24 to Sunday, February 26, 2023, a weekend built on the pillars of what The Alliance does: Help. Support. Recovery. Join this national movement, as we ensure that NOT ONE MORE life is lost, NOT ONE MORE child is taken, and NOT ONE MORE precious moment is destroyed by this insidious disease. Over this three-day weekend, help us continue to raise awareness and offer direct support to individuals and families across the country. Proceeds from the NOT ONE MORE Weekend will directly fund our free, weekly, virtual eating disorders support groups!
EATING DISORDERS AWARENESS WEEK: IT’S TIME FOR CHANGE
JOIN THE EDGI STUDY TODAY
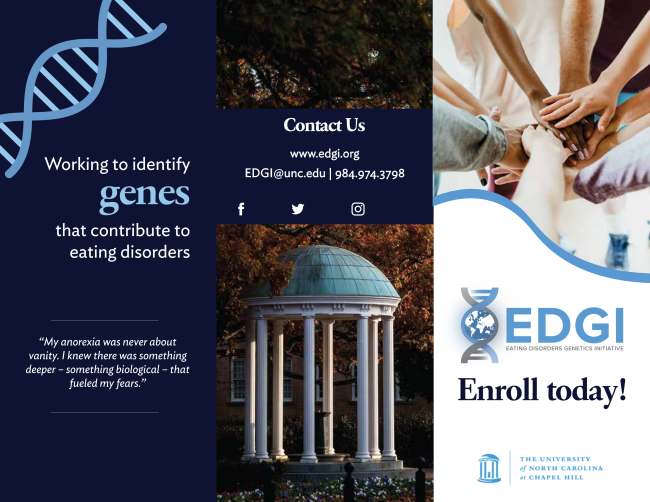
The Eating Disorders Genetics Initiative (EDGI) is the largest-ever genome-wide association study for eating disorders. EDGI will create the blueprint to identify the causes of anorexia nervosa, bulimia nervosa, and binge-eating disorder. The Eating Disorders Genetics Initiative (EDGI) is an international research study designed to understand how your genes can influence your risk for developing an eating disorder.
You can help by introducing the study to your patients. The goal is 6000 participants. See the 5 simple steps (below) for participation. There is also a link below to download a flyer for your waiting room, post on your website or blog, or send to clients electronically,
We know that one treatment doesn’t fit all eating disorders. EDGI will guide us toward a personalized medicine approach including tailored treatment and recovery plans. EDGI will allow us to understand how both genes and environment influence risk for these disorders. The purpose of EDGI is to learn more about how genes influence risk for bulimia nervosa, binge-eating disorder, and anorexia nervosa. By introducing this important study to your patients, you can help advance understanding of the genetics of eating disorders and contribute to a future with better treatments!
You can download the flyer (above) to share here.
ONLINE DONATIONS NOW ACCEPTED TO COPE

Dear COPE FRIENDS,
Great news! Our Donation icon now allows you to use PayPal to charge your contribution to the credit card of your choice. It is safe, secure and you can rest assured your donation will be supporting the community outreach, education, and scholarship funds that help us help our community.
Everyone knows someone who is struggling with an eating disorder, body image distress or other disordered eating challenges. COPE has been active in Volusia and Flagler counties since 2001, dedicated to make a difference. We are involved in the local schools, colleges, community health forums, lobbying in Washington, D.C. for legislative change, speaking across the area and now proud to offer scholarship funds for those who would not be able to receive essential health care.
All of us involved in COPE: Community Outreach for the Prevention of Eating Disorders, are dedicated volunteers, working to eliminate eating disorders, improve body image and restore peace and balance to those affected by these life threatening challenges. We have been a community resource, and 501©(3), Jan. 2001.
COPE provided many resources that are a beacon of hope for those who suffer or have loved ones affected by eating disorders and body image issues.
Our Mission
Our focus is to provide up-to-date learning resources via outreach, media attention, and community events; we strive to educate our local community in order to facilitate greater understanding and more effective approaches to treating eating disorders and improving body image.
Scholarships for treatment are available for our local community members (Volusia and Flagler counties).
For information and applications for scholarship opportunities:
Contact: Kathryn Fraser, Ph.D. at [email protected]